October being Breast Cancer Awareness Month, we bring you the latest updates on our country’s most common cancer in women, plus inspiring stories from survivors By ELIZABETH LIEW

October being Breast Cancer Awareness Month, we bring you the latest updates on our country’s most common cancer in women, plus inspiring stories from survivors By ELIZABETH LIEW
THE NUMBERS:
The Singapore Breast Cancer Foundation (BCF) conducted a survey*, and this is what they found:
More than 75% of Singaporeans admit to having limited knowledge of breast cancer.
Only 2 in 5 women under 45 years old perform any form of medical breast checks, such as mammograms.
45% of women perform regular self-examinations and go for medical checks, while 27 per cent have never checked.
*Statistics from the Breast Cancer Foundation’s Annual Report 2017-2018.
Breast cancer is not only one of three cancers in women here, it’s also the top killer. “One out of every 17 women in Singapore is likely to be affected by breast cancer in her lifetime,” reveals Dr Esther Chuwa, Consultant breast and General Surgeon at Gleneagles Hospital. On average, more than 1,900 new cases of breast cancer are diagnosed annually in Singapore. Between 2011 and 2015, 9,634 women were diagnosed with breast cancer, with 2,105 fatalities**.
“Over the past 40 years, the rate of breast cancer has almost tripled. But the good news is that women diagnosed in stage one have a 91 per cent chance of surviving beyond five years, compared with only 20 per cent for those discovered at stage four. Hence, the message of screening and early detection can never be emphasised enough.”
WHAT’S YOUR RISK?
A new study found that women who have inherited a mutated BRCA gene, such as actress Angelina Jolie, have an increased cancer risk. “BRCA genes function to repair cell damage and keep breast, ovarian and other cells growing normally,” Dr Chuwa explains. “But when these genes are mutated, the cells don’t function normally, thus increasing the risk of cancer.”
Women who have a BRCA1 mutation have up to an 80 per cent lifetime risk of being diagnosed with breast cancer and up to a 60 per cent lifetime risk of ovarian cancer. Women with a BRCA1 or BRCA2 mutation also have an increased risk of developing ovarian, colon and pancreatic cancers, as well as melanoma (skin cancer). “However, only about five to 10 per cent of breast cancers are thought to be hereditary or caused by abnormal genes passed from parent to child,” Dr Chuwa says, which means the vast majority of women who develop breast cancer don’t have a family history of the disease.
Other risk factors include:
• Previous breast biopsy showing atypical hyperplasia, an accumulation of abnormal cells or lobular carcinoma in-situ, when they form in the milk glands (mammary glands) in the breast.
• Early menstruation (i.e. before the age of 12) and late menopause (i.e. after the age of 55).
• Having your first child after the age of 30.
• Regular consumption of alcohol.
• Long-term use of combined hormone replacement therapy.
• Obesity especially following menopause.
Take steps to actively lower your risk, such as exercising more to maintain a healthy weight, as well as eating fresh fruits and vegetables and cutting down on processed food and red meat. “These won’t stop you from getting breast cancer but it will reduce the risk and detect any abnormalities early,” Dr Chuwa says. Importantly, check your breasts regularly on a monthly basis and go for a mammogram once a year once you’ve reached 40.
She notes, “The earliest stage of breast cancer usually produces no symptoms and can only be detected on screening mammograms or through breast ultrasounds.”
THE RISE OF GENETIC TESTING
For some women with a family history of breast cancer, genetic testing is a way of being proactive about their health. It allows them to determine their risk of developing cancer in the hope that they can change the outcome. “A comprehensive genetic testing panel via a blood sample can assess if these genetic mutations are present,” Dr Chuwa says, “but these tests are costly and may not be necessary for everyone.” She also stresses that having a negative test does not mean that you are immune from the more common non-hereditary breast cancer, which is clearly evident from Tracy’s story (see story on the right).
WHAT ARE THE LATEST TREATMENT TRENDS?
“The gold standard to diagnose breast cancer is through a tissue biopsy,” Dr Chuwa says, a procedure that involves inserting a needle into the area of abnormality to remove the material and examine it under a microscope.
Treatments have improved over the years, which has helped to keep the death toll fairly stable despite the rise of incidence, Dr Chuwa affirms.
“In the past, doctors would treat breast cancers according to the stage of the disease – how large the cancer is, if there is cancer spread beyond the breast. While this is still vital, doctors are increasingly recognising the importance of cancer biology: That breast cancer cells have highly varied behaviour based on the genes the cancer expresses. For instance, the outcomes of a stage one indolent cancer and that of a stage one aggressive cancer differ greatly.” Medical advancements mean doctors can now analyse and tailor treatments to these cancer cell behaviours to optimise outcomes, Dr Chuwa reveals.
**According to the latest cancer registry report released in June 2017.
HOW TO CONDUCT A BREAST SELF-EXAMINATION (BSE)***
Begin by lying on your back and place your right hand behind your head. With the pads of the middle, index and ring finger of your left hand, gently yet firmly press down using small motions to examine the entire right breast, ensuring you’ve covered all the breast tissue. Next, sit or stand and feel your armpit because breast tissue extends to that area. Gently squeeze the nipple, checking for discharge. Repeat the process on the left breast. Now, stand in front of the mirror with your arms by your side. Look out for the signs of breast cancer, which include:
1. A painless lump in the breast or armpit.
2. Rashes around the nipple.
3. Discharge from the nipple.
4. Changes in the skin over the breast and nipple.
5. Retraction (pulling in) of the nipple.
If you find changes or anything new in consecutive self-examinations, highlight it to your doctor right away.
***Adapted from The Singapore Breast Cancer Foundation

Use fingerpads with massage oil or shower gel

Up and down
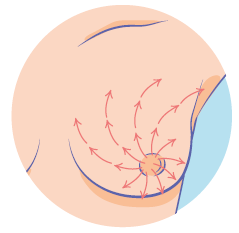
Wedges

Circles
“I could be dead in one to two years if I didn’t go for the checkup” – Phyllis Cheong, 38
A few months after being diagnosed with depression in 2017, Phyllis was diagnosed with stage two breast cancer. She found a lump on her breast in June, but waited six months to get it checked. “I was working in Hong Kong at the time but I wanted to do the check-up in Singapore. When the results came back, luckily, I was still in the early stages of breast cancer, but if I had seen a doctor six months earlier, I would have been at stage one.”
“Upon receiving the diagnosis, my mind went blank and it seemed like a nightmare. Breast cancer was something I knew about vaguely, but I knew I had to accept the fact and deal with it.” After relocating back to Singapore, she underwent six gruelling months of chemotherapy. “It was a wakeup call for me,” she shares, “but I love my parents and don’t want them to worry about me, so I needed to get well!”
Despite the tough treatments, Phyllis persisted, thanks to the support of family and friends, and continued living life normally. “Of course, I tried to eat healthier, avoided raw food and switched to using products with natural ingredients.”
“To take my mind off cancer and the pain, I turned to painting, and I plan to sell some of my paintings to raise funds for the breast cancer cause*. I’ve also set up a bucket list of things to do as soon as I am well, which mostly involves seeing the world. I want to learn diving, take my mum to Japan, ride on a hot air balloon and travel Europe and South America.”
After her chemo ended, Phyllis attended a BCF support group and met other survivors, some of whom have been in the group for 20 years. “It gives me hope and I would absolutely encourage other breast cancer survivors and caregivers to join us.”
Phyllis had a lumpectomy on July 31 this year and she’s still recovering but is considered cancer-free. “I treasure life so much now because you only live once, and I could be dead in one to two years if I had not gone for the checkup. My motto is ‘live in the present and enjoy life to the fullest’. Forget about bad things that happened in the past and forgive.”
She hopes to become a good artist and home decorator and set up her own company. “Don’t let cancer defeat you,” she says. “Looking back at what I’ve endured, it was tough but I did it. You can come out a stronger and happier woman. Appreciate every single beautiful thing that happens around you. There is always life after breast cancer.”
Phyllis’ words of advice: “Breast cancer does not discriminate; it is important for every woman to take charge of her breast health. Don’t wait to do self-checks and consult a doctor if you find anything such as a lump or nipple discharge.”
*Phyllis is holding a fundraising event at Sideways Café on October 13. Visit www.artbylissylove.com for more information.
COLOUR YOURSELF PINK
Show your support and raise funds for the Breast Cancer Research Foundation with these limited edition picks

Origins Hand and Mind Relief Set (Plantscription Anti-Aging Hand Cream & Peace of Mind Rollerball), $29.

Estée Lauder Limited Edition Advanced Night Repair with pink ribbon keychain, $175 (50 ml).

La Mer The Cleansing Micellar Water, $95 (100 ml).
Clinique Great Skin, Great Cause Dramatically Different Moisturising Lotion+ with charms, $85 (200 ml).

Bobbi Brown Pinks with Purpose Lip Color Duo (Sandwash Pink & Pink), $66.

“If I can go through chemo, I can go through anything” – Tracy Hoon, 31, Office Manager, Financial Services Job Board
When Tracy’s aunt got diagnosed with stage three breast cancer in August 2016, it made the 29-year-old realise she should get checked. “I went home and did a self-examination. That’s when I felt something protruding on my right breast.”
Just two weeks later on August 30, Tracy was diagnosed with stage two to three breast cancer, which had spread to a few lymph nodes. “I cried, because I couldn’t believe it. At age 29, going for mammograms and anything to do with breast cancer was the last thing on my mind. I was definitely not within the at-risk group; I don’t smoke or drink alcohol, I don’t have a family history of breast cancer (my aunt and I both did genetic testing and it was negative) and I’m not above 45 years old.”
“My first thought was ‘Why me? I’m so young and I’m not prepared to die yet; I still have a lot of things to do.’ I had just got married in November 2015, just moved into my new BTO flat and just started a new job. Everything was falling into place and then this happened. I didn’t know how to break the news to my parents because I felt a strange sense of guilt. Did I not look after myself enough? I’m supposed to look after them till they’re old, but I didn’t know if I would even survive this illness.”
Tracy started six months of chemotherapy in September 2016, persevering in spite of side effects like insomnia and joint pains. “I never thought about giving up because my mind was so focused on needing to get well. Obviously, one of the more emotional aspects of chemo was losing my hair, but it’s really nothing compared to getting well. Hair grows back and I told myself to just be strong.”
She also picked up hobbies like calligraphy and making clay jewellery, as well as joined a support group at the BCF with her husband (he would go for the Caregivers support group). “Seeing survivors of 10, 15 years there gave me hope that there’s life after cancer.”
“After going through chemo and everything, I learnt to appreciate life and the people around me. I used to be a grump, complaining about everything under the sun and getting easily affected by what others said about me. Now, I’m more happy-go-lucky,” Tracy reveals. She is now a vocal advocate for creating awareness among younger women and is working with the BCF’s young women’s support group.
In March 2017, Tracy had a mastectomy to remove her right breast tissue and replace it with belly fats. “I kind of love my body now. My battle scars remind me that I’ve survived and I’m a warrior with a story to tell.”
Tracy’s words of advice: “If I can have breast cancer at 29, then you should do your checks too. The earlier it’s discovered, the better your treatment options and the higher your chances of survival too.”

“I want to see my kids grow up and get married” – Sharon Phua, 46, Counter Retail Manager
“In early February 2013, I felt a lump in my right breast, just below my armpit,” Sharon recounts. Then just 41 years old, the mother-of- three felt calm as she had just gone for a breast check in October 2012 and results were all clear. “I delayed seeing a doctor until April, and was referred to a specialist at SGH (Singapore General Hospital) who did a biopsy and confirmed that I was at the first stage of breast cancer.”
“I was devastated, and my immediate concerns was wondering how much time I had left and who would take care of my three children, who were 21, 20 and 12 years old, if I was no longer around. I still want to see my kids grow up and get married, I still want to see my grandchildren. I actually cried almost every night. Another concern was the financial burden of my treatments, but my family and company insurance helped me through.”
Sharon was reluctant to go for chemotherapy at first. “I was scared because I heard it’s torture and there are side effects, like my hair would drop and my body would become weak. But through the encouragement of my family members, church friends, boss and colleagues, I took up the challenge and shaved all my hair off.”
Her husband, Adrian, was her rock throughout her cancer battle, and gave her the courage and strength to persevere. “I was on sick leave for a year and Adrian was always by my side 24/7, accompanying me for all my medical checks and treatments.”
She underwent chemo and radiotherapy for about one year and was officially declared cancer-free in 2016. “This tough journey changed my whole attitude towards life. I love and appreciate myself and my family more, and I can now share my experiences with others who are going through the same thing. Now I go to yoga and gym more often, and spend more time with my family.”
Sharon’s words of advice: “There’s a quote that I love: ‘You will never know how strong you are until being strong is the only choice you have’. You don’t really have a choice when you’re diagnosed with cancer, but always believe in miracles and a hope for a cure.”

The Pink Ribbon Walk organised by the BCF will take place on 6 October to raise funds and awareness for breast cancer.
This year’s theme is “Every Woman Matters”. Visit www.bcf.org.sg for more information.

FACT OR MYTH
Dr Chuwa breaks down some common breast cancer beliefs
1 If breast cancer runs in the family, the chances of getting it are higher.
FACT. Having one or more close relatives with breast cancer does increase your risk. If you’ve had one first-degree female relative (sister, mother, daughter) diagnosed with breast cancer, your risk is doubled. If two first-degree relatives have been diagnosed, your risk is five times higher than average.
2 Handphones and other wireless equipment like microwaves or even mammogram machines can cause breast cancer.
MYTH. Low-energy radiation, including cell phone signals, microwaves and Wi-Fi, does not have enough energy to effect DNA damage. Of note, mammograms expose the breasts to tiny amounts of radiation. Modern machines use low radiation doses to get breast x-rays with high image quality. The benefits of mammography in detecting early stage breast cancers far outweigh any possible harm from the radiation exposure.
3 Wearing underwire bras causes breast cancer.
MYTH. It is believed that underwire bras restrict the drainage of toxins from the breast, resulting in accumulation of cancer-causing substances in the breast. However, a scientific study found no real difference in the risk between women who wore a bra and those who didn’t. With that said, being overweight increases breast cancer risk and is associated with women having larger breasts and needing to wear a bra more often, so the risk lies in the woman’s weight instead of the underwire bras.
4 If I have breast cancer, I need to have a mastectomy.
MYTH. Surgery has progressed considerably over the last few decades. There is more emphasis on preserving a good functional quality of life as the women now survive longer with better drugs, and there’s a trend towards reconstructive and oncoplastic surgical approaches that better preserve the shape and form of the breast despite cancer removal.
5 A lump in my breast is a symptom or early stage of breast cancer.
MYTH. The most common symptom of breast cancer is a lump in the breast. However, 90 per cent of breast lumps felt by women are benign. It is important to be vigilant, but do not panic. Observe if the lump resolves following menstruation; if it persists, consult your doctor who will order tests like an ultrasound scan to determine the nature of the lump.























